1. Specialists Involved
Diagnosing aplastic anemia often involves a team of specialized healthcare professionals working together to ensure accurate assessment and treatment planning.
- Hematologists: Hematologists are crucial for diagnosing aplastic anemia, as they specialize in blood and bone marrow disorders. They thoroughly assess patients, interpret lab results, and formulate treatment plans tailored to each individual.
- Clinical Pathologists: These specialists analyze laboratory tests and bodily fluids, such as blood and bone marrow samples, to identify abnormalities in blood cell counts and other markers that indicate aplastic anemia.
- Oncologists: Oncologists, who specialize in cancer and various blood disorders, may be involved to rule out conditions like leukemia or myelodysplastic syndromes that present similar symptoms. Their expertise ensures a comprehensive evaluation, helping to differentiate between benign conditions like aplastic anemia and more serious diseases.
2. Medical and Family Histories
A detailed medical and family history is essential to understanding potential risk factors and causes.
- Medical History: Healthcare providers explore the patient’s past illnesses, treatments, and medications that might contribute to bone marrow suppression, such as chemotherapy or specific antibiotics. Exposure to toxins like benzene or radiation can also be relevant.
- Family History: Some cases of aplastic anemia are influenced by genetic factors. Inherited bone marrow failure syndromes, such as Fanconi anemia or dyskeratosis congenita, can predispose individuals to the condition. Recognizing familial patterns helps guide genetic counseling, preventing potential transmission within families.
- Lifestyle Factors: Lifestyle habits, including smoking, alcohol consumption, and chemical exposure at work or home, can provide additional insight into triggers for aplastic anemia. Documenting these factors helps clinicians develop informed diagnostic and treatment strategies.
3. Physical Exam
A thorough physical examination provides essential insights and clues for diagnosing aplastic anemia.
- Skin and Mucous Membranes: During the exam, physicians assess the skin for bruising, petechiae (small red or purple spots), and pallor, all common in individuals with low blood cell counts. Mucous membranes are also checked for similar signs.
- Signs of Bleeding or Infection: Healthcare providers look for signs of bleeding or infection, as these may indicate compromised bone marrow function. They may also check for an enlarged lymph node or spleen and assess abdominal areas for abnormal swelling or tenderness.
- Neurological and Vital Sign Assessment: Evaluating vital signs, such as heart rate and blood pressure, provides clues about the condition’s severity. Additionally, a neurological exam may be performed to detect fatigue or muscle weakness, suggesting anemia-related complications.
4. Diagnostic Tests
Several diagnostic tests confirm aplastic anemia and help determine its severity.
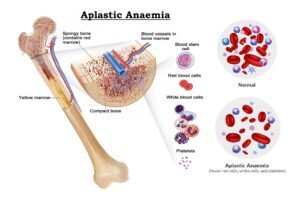
- Complete Blood Count (CBC): This test measures red blood cells, white blood cells, and platelets. In aplastic anemia, the CBC often shows pancytopenia, a significant reduction across all three blood cell types, which provides insights into the extent of bone marrow suppression.
- Peripheral Blood Smear: A peripheral blood smear examines the size, shape, and count of blood cells under a microscope. Abnormalities, such as macrocytosis (enlarged red blood cells) or leukopenia (reduced white blood cells), help differentiate aplastic anemia from other blood disorders.
- Bone Marrow Aspiration and Biopsy: These procedures provide critical information about bone marrow health. In a bone marrow aspiration, liquid marrow is extracted and analyzed for cellularity, often showing a reduced number of hematopoietic (blood-forming) cells in aplastic anemia. A biopsy further evaluates the marrow’s structure and cell types.
Conclusion
Diagnosing aplastic anemia is a complex process that involves a multi-disciplinary approach, requiring insights from hematologists, pathologists, and oncologists. By gathering medical and family histories, conducting a comprehensive physical exam, and utilizing diagnostic tests, healthcare providers ensure an accurate diagnosis and tailor treatment plans to improve patient outcomes.
This collaborative approach is vital in addressing not only the symptoms but also the underlying causes of aplastic anemia. Ongoing advancements in medical research and diagnostic tools continue to enhance the prognosis for patients, offering hope for improved outcomes and a better quality of life. Early detection and intervention are key to helping individuals with aplastic anemia live fulfilling lives.